Making Every Moment Count:
How Treatment Options for Metastatic Breast Cancer Could Improve the Patient Experience
UNDERSTANDING THE PATIENT EXPERIENCE
“I try to be strong, and I try to be independent. So far, I’ve been able to do that, even at [the cost of] sacrificing my time and energy.” Amy D., a wife and mother living with metastatic breast cancer, receives various methods of treatments on a monthly basis to manage this disease.
For people with incurable metastatic breast cancer (MBC), time is precious. Yet current treatment options can bring their own set of difficulties that can make managing this disease challenging for patients. This can include having to re-prioritize personal and professional commitments due to "time toxicity": the time it takes to undergo cancer-related medical care, including travel and wait times.1 Collectively, this takes away from valuable aspects of a patient’s daily life such as pivotal moments with family, friends, colleagues and a number of other responsibilities. With a variety of treatment options, patients have the chance they deserve to choose methods that will best fit into their life and take back time to focus on themselves – not their disease.
To take a closer look at this and better understand the needs of patients with MBC, Ipsos and Living Beyond Breast Cancer (LBBC) co-authored a recent survey funded by Eli Lilly and Company. 100 female ER+, HER2- patients with MBC in the U.S., who had not previously received an intramuscular (IM) SERD as part of their treatment, were surveyed to identify opportunities to advance care, improve patient experience and highlight the importance of what treatment options could mean for people living with MBC. The survey found that time and transportation were both significant barriers for respondents that negatively impacted other areas of their lives.
DIVING DEEPER: PATIENTS WITH MBC
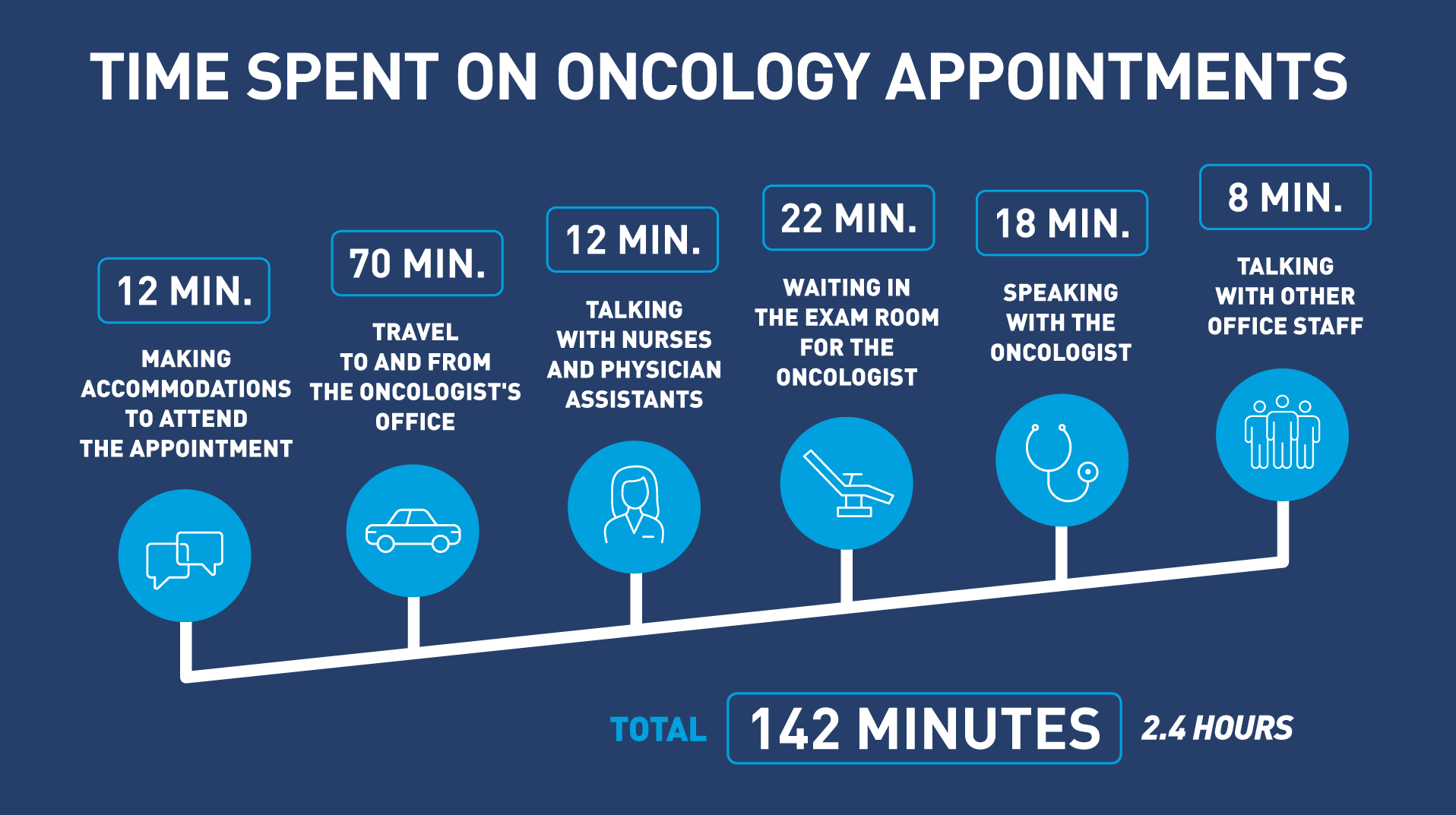
The survey found that, on average, medical appointments take more than 2 hours per visit, including travel, wait times and treatment. Often, recovering from treatments can take even more time away from daily activities that bring normalcy and joy to the lives of patients. Respondents shared in the survey that this can include exhaustion, anxiety or other physical and emotional impacts that further contribute to time toxicity.
One patient with MBC, Stephanie W., shares her insight into how managing MBC has impacted how she spends her time. “When you calculate all the time it takes… over a period of time like I have, I’ll never get those hours back. What I could have done with that time… could have been extra time with my husband or making memories with my grandkids.”
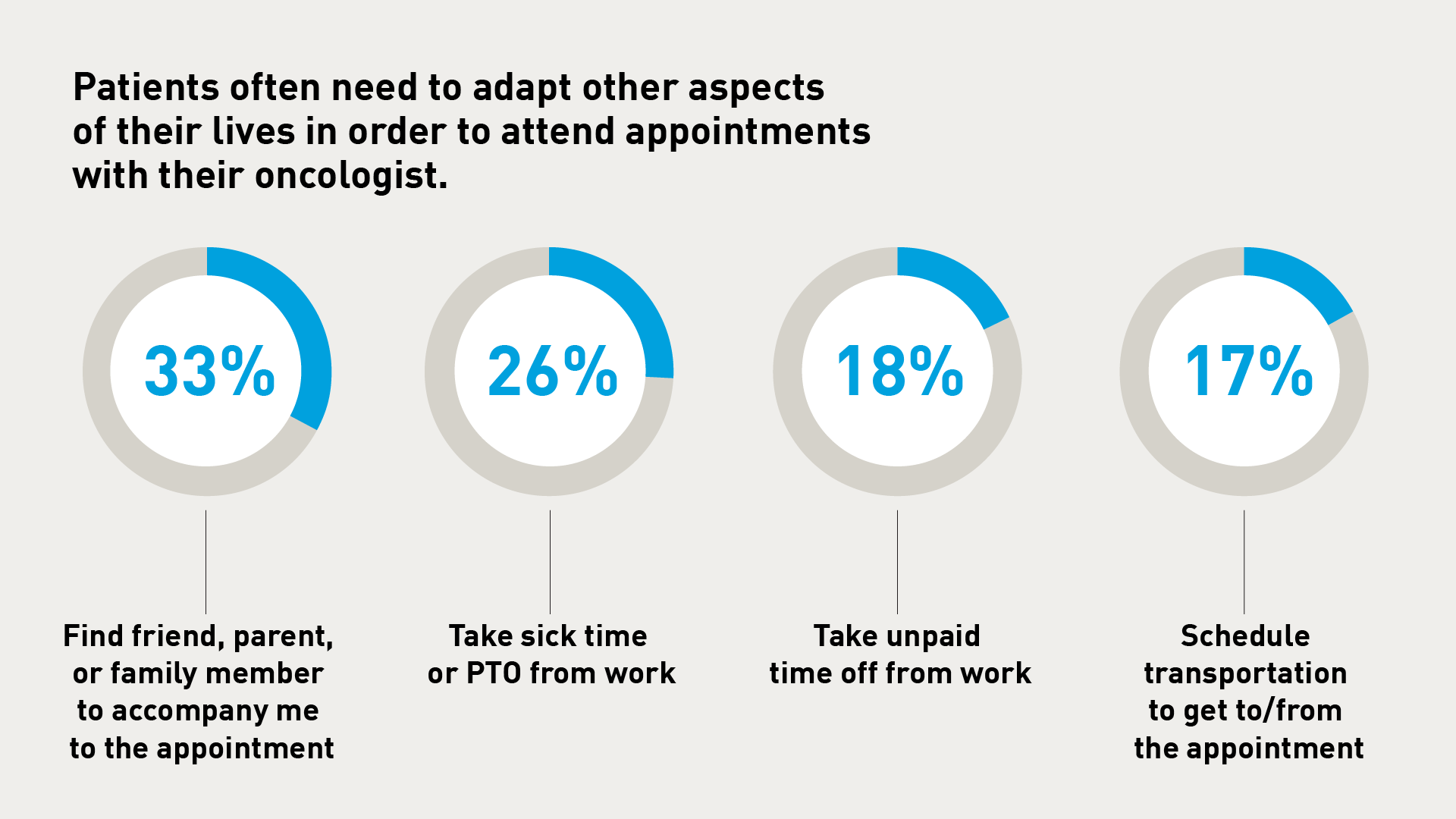
Additionally, MBC management methods can create other demands for those living with the disease, such as requiring them to take unpaid time off for appointments, arranging transportation to and from office visits, as well as arranging childcare, if needed.
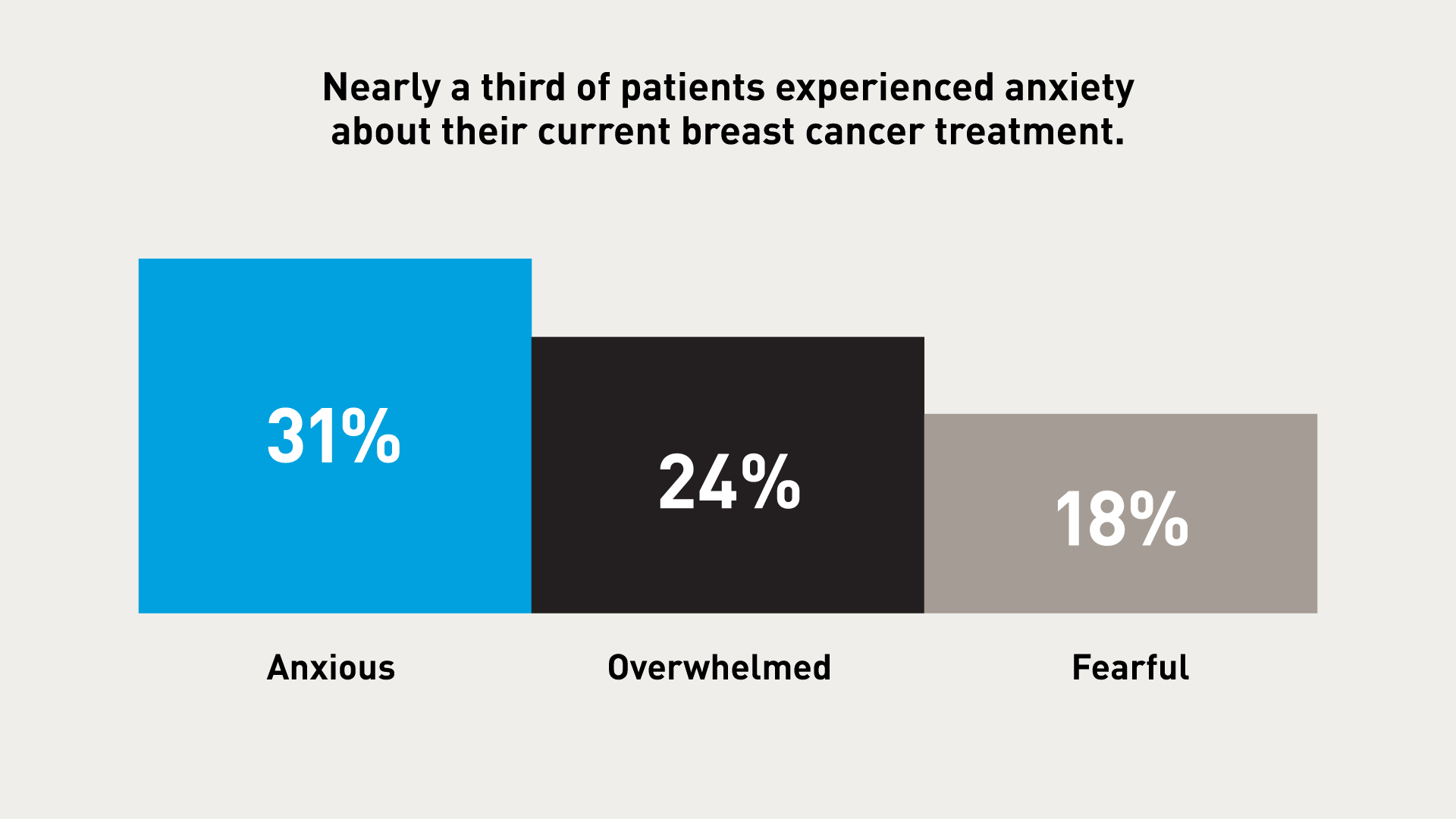
This high demand on time for those with an incurable disease can lead to an increase in anxiety, fear and the feeling of being overwhelmed – adding additional strain to the disruption this disease has already caused in the lives of patients.
Amy D. offers her perspective on the emotional impact of her treatment journey. “When you don’t know how much time you have left, it makes the world stop.” Learn more by watching Amy's story below.
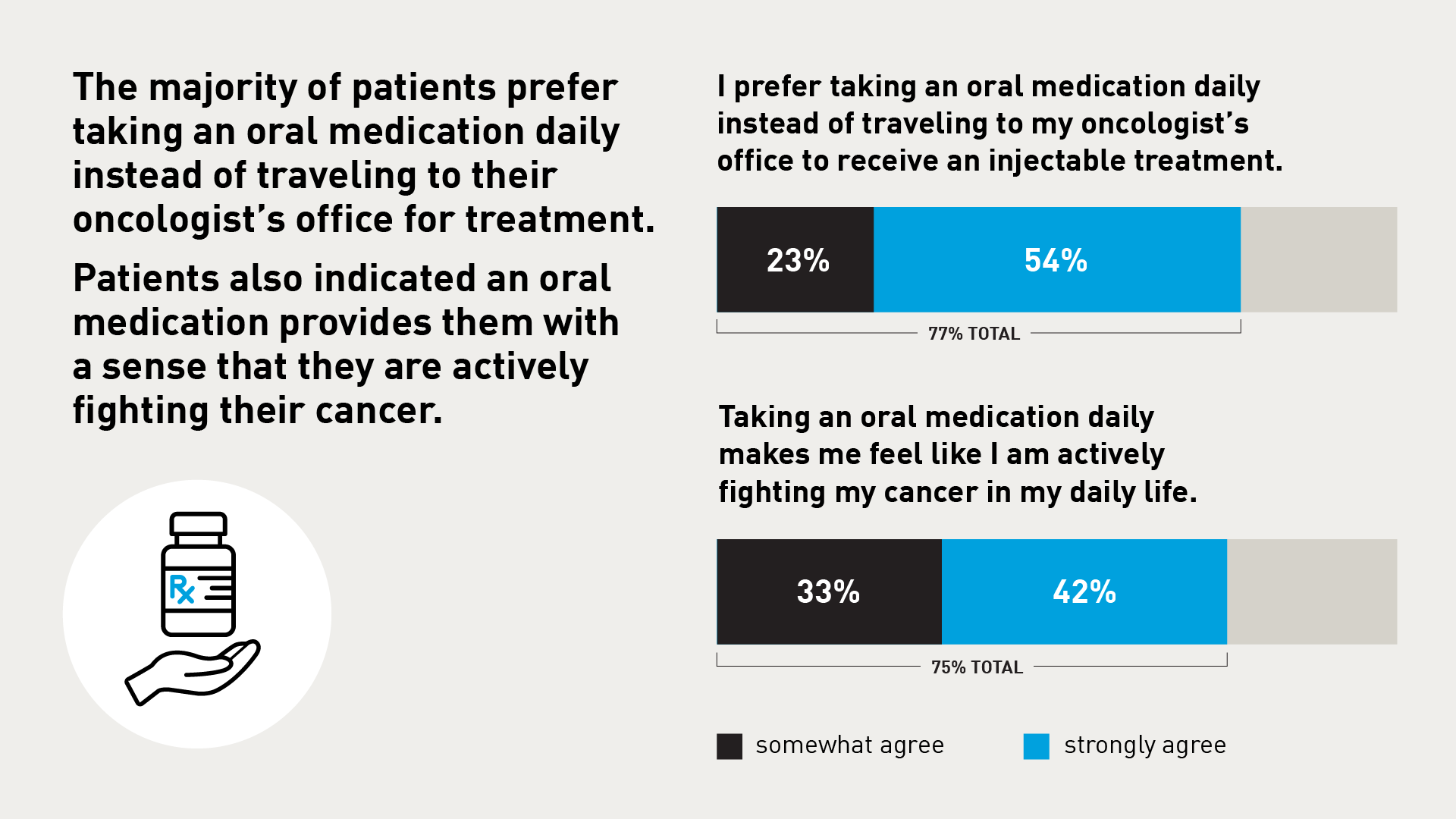
The possibility of additional treatment options is one potential way to reduce time toxicity, according to the survey. For instance, some medications require monthly in-office visits for IM injections. Patients say oral medications that could be taken at home could help cut down on time spent receiving treatment and give them much needed space to pursue the activities and relationships that make their lives more vibrant.
An oral treatment option gives patients a sense of control over their lives and empowers them to actively fight cancer without affecting or interrupting their routine. These seemingly simple benefits weigh heavily for patients when evaluating breast cancer treatments.
PATIENTS DESERVE OPTIONS
Hear the stories of two patients with MBC and the ways in which their treatment has affected their lives below.
Amy D.
Stephanie W.
Having worked with patients in the MBC community for 10 years, I have witnessed the impacts that treatment can have on the lives of patients, including the time burden to receive treatment, as well as physical and mental impacts. The availability of new treatment options could give patients more control over their time.
Sonya Negley
Executive Director, METAvivor
THE POWER OF TIME
Patients with MBC already deal with the weight of an incurable disease, making it important to understand what can be done to lighten the load for them. Potential oral treatment options may give back some of that precious time to patients so they can spend time with people they love, do the things they enjoy and focus on themselves and their well-being.RESOURCES
About MBC
Metastatic breast cancer is a cancer that has spread from the breast tissue to other parts of the body. Local or regional metastatic breast cancer means the cancer has grown outside the organ where it started but has not yet spread to other parts of the body.2
Of all high risk early-stage breast cancer cases diagnosed in the U.S., approximately 30% will become metastatic3 and an estimated 6-10% of all new breast cancer cases are initially diagnosed as being metastatic.4
Survival is lower among women with a more advanced stage of disease at diagnosis: five-year relative survival is 99% for localized disease, 86% for regional disease and 30% for metastatic disease.5 Other factors, such as tumor size, also impact five-year survival estimates.5

*The survey was conducted online by Ipsos in partnership with LBBC and funded by Eli Lilly and Company. The survey was conducted August 23 to October 18, 2023. Read the full survey results here.
1. Rossi, M. (2023, August). The Time Toxicity in Cancer Patient. PubMed | National Institute of Health. https://pubmed.ncbi.nlm.nih.gov/37392102/. Accessed January 19, 2024.
2. American Cancer Society. Understanding Advanced Cancer, Metastatic Cancer and Bone Metastases. https://www.cancer.org/treatment/understanding-your-diagnosis/advanced-cancer/what-is.html Accessed January 19, 2024.
3. Lee, Viv. “Types of Breast Cancer: Metastatic Breast Cancer.” BreastCancer.Org. 2024. www.breastcancer.org/types/metastatic. Accessed January 11, 2024.
4. National Library of Medicine. The Clinicopathological Features and Survival Outcomes of Patients with Different Metastatic Sites in Stage IV Breast Cancer. National Institute of Health. 2019. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6852913/. Accessed January 11, 2024.
5. American Cancer Society. Breast Cancer Facts & Figures 2022-2024. Atlanta: American Cancer Society, Inc. 2022. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/breast-cancer-facts-and-figures/2022-2024-breast-cancer-fact-figures-acs.pdf. Accessed January 19, 2024.





